What are the Potential Benefits of Taking Collagen During Pregnancy?
Pregnancy is characterized by physiological changes, such as increased plasma volume and red blood cells, but serum protein levels are below normal in many women. The maternal diet during pregnancy directly impacts the fetus's health, and the pregnant woman's protein needs skyrocket from 46 g to 71–76 g per day, according to the study in the Journal of Pregnancy and Child Health(1).
The study showed an improvement in blood protein levels in 100% of women receiving collagen, with 94% reaching above 6.6 g/dL at 6 weeks postpartum (64% in the control group). At week 10, this rate was 86% in the collagen group and 50% in the control group. Furthermore, the collagen significantly improved physical health and quality of life (WHOQOL-BREF scale).
Pregnant women's bodies produce collagen, which may have important roles in immune tolerance, angiogenesis (the creation of new blood vessels), and spiral artery remodeling, according to another study in the International Journal of Biological Sciences(2).
The study also suggests that fetal membranes (amnion and chorion) primarily consist of collagen and that their structural strength and integrity play a crucial role in the maintenance of pregnancy and childbirth. An imbalance between matrix metalloproteinases (MMPs) and their inhibitors (TIMPs), which impact collagen degradation, may be linked to premature membrane rupture.
Are There Risks Associated with Taking Collagen While Pregnant?
Studies showing the side effects of collagen supplements in pregnant and postpartum women did not report any serious adverse events(2). Mastitis, depression, disorders of the reproductive system and the breast, kidney, and urinary tract problems, and urinary tract infections were the most frequently reported adverse events in the scientific study.
However, as these events were also reported in the control group and the overall rates of adverse events were similar between groups (29.6% in the control group, 27.0% in the collagen group), it was concluded that these events were not directly related to collagen supplementation. Meanwhile, pregnant women who take collagen supplements run the risk of experiencing the following side effects.
Lack of Extensive Research
Collagen supplement research has been heating up recently, particularly since 2019. Although collagen supplements have been the subject of extensive scientific research, there is currently an insufficient number of studies conducted on pregnant women.
Potential for Low-Quality Supplements
Ingredients of inferior quality in collagen supplements may induce severe health complications and pose hazards during pregnancy. There are a lot of problems that pregnant or nursing women can experience from using low-quality marine collagen or fish that are heavy in mercury or other metals. In addition, pregnant women may experience a variety of adverse effects from collagen supplements that are not naturally fed to bovine collagen strains and are supplemented with antibiotics.
Allergies or Sensitivities
Pregnant women were compared with non-pregnant individuals, and no significant differences were observed between the two groups in terms of gastrointestinal disorders (e.g., abdominal pain, hemorrhoids) and skin and subcutaneous tissue disorders (e.g., itching, allergies, sensitization)(2). It may not be right to apply these results to all collagen supplements, given that they are type-specific.
Interactions with Other Medications
As a dietary supplement, collagen is typically safe to take alongside most prescription drugs. Yet, before taking collagen supplements, you should talk to your doctor about any health issues you may have, like allergies, hypertension, sensitivity, or nausea. Taking collagen supplements, particularly those derived from fish, bovine, or any other animal, can trigger an allergic response in certain people.
The hydrolyzed form of collagen is the most easily digestible supplement form. However, some medications (such as calcium channel blockers and thyroid medications) may have their absorption affected by certain foods, so it is best to avoid taking these with those medications. To lessen the likelihood of drug interactions, take collagen supplements at least a few hours before or after taking medications.
When to Avoid Collagen During Pregnancy
Collagen supplements during pregnancy appear to be generally safe; however, it is advisable to consult your physician beforehand. Show the label and check the ingredients. You might have to be cautious or not use it at all in certain situations:
- Be sure to consult your physician in the event that you encounter any complications while pregnant, such as pre-eclampsia, gestational diabetes, or any other health issue. These conditions may have some complex connections with collagen.
- If you use fish-sourced collagen, there may be risks, such as mercury, especially if you don't know the source. Bovine collagen may be a less risky option.
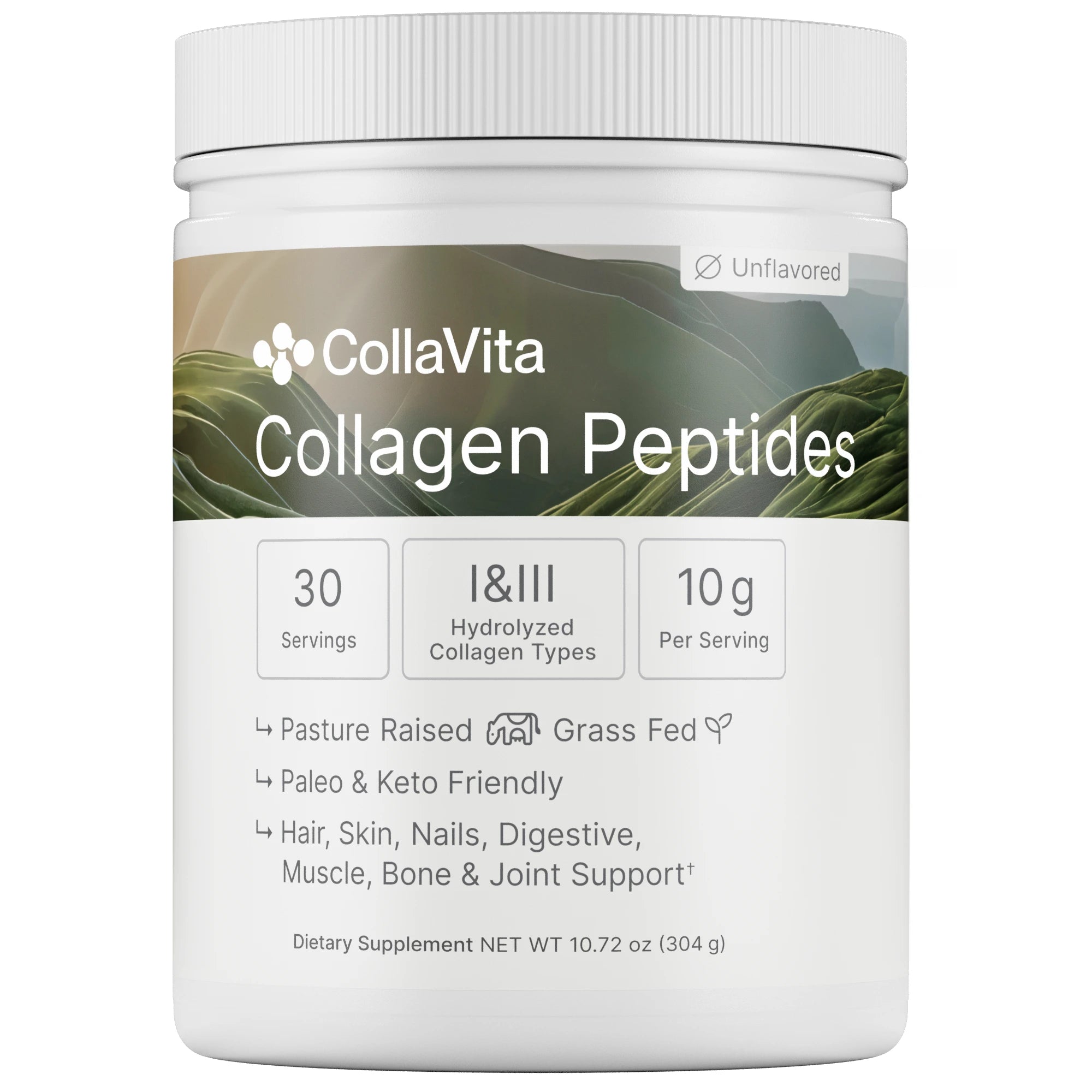
- Avoid products of poor quality or unclear ingredients. It is important to choose trusted brands.
- If you take regular medications, talk to your doctor about how collagen interacts with them.
Which Type of Collagen Should You Choose During Pregnancy?
During pregnancy and nursing, there is a significant rise in the demand for essential proteins. For optimal skin and internal organ health, it is essential to take Type-1 and Type-3 collagen supplements during this time. However, type-2 collagen supplements can help reduce some of the strain on pregnant women's cartilage structures.
Types of collagen can be of bovine or marine (marine/fish) origin. On the other hand, it is safer for fetal development to take collagen supplements, particularly those that do not contain tryptophan and have low levels of harmful amino acids.
To further reduce the likelihood of gastrointestinal issues during pregnancy, it is best to use peptides with a low molecular weight.
How to Incorporate Collagen Safely into Your Pregnancy Diet?
Collagen, a vital protein that supports skin elasticity, joint health, and tissue repair, may offer benefits during pregnancy, such as reducing stretch marks and supporting joint comfort. However, safety is paramount when adding collagen take to your diet while expecting. Below, you will discover a list of important things to think about when incorporating collagen supplements into your regular regimen.
Recommended Dosage (if any)
A general rule of thumb, not an absolute one, is to take 10-15 grams of collagen supplement daily. To find out how much you should take, it is important to talk to your doctor. They can assess your unique nutritional needs and help you develop a healthy plan for your pregnancy.
Best Ways to Consume Collagen (powders, drinks, etc.)
Depending on your preferences and way of life, you can choose from a variety of convenient collagen forms:
- Powders: Versatile and easy to incorporate, powders can be mixed into smoothies, soups, or even water. They’re ideal if you enjoy customizing your intake.
- Capsules: Perfect for those who prefer a tasteless, no-fuss option. Capsules are portable and require no preparation.
- Drinks: Pre-made collagen drinks offer convenience for busy schedules, making them a great on-the-go choice.
For optimal absorption, look for hydrolyzed collagen when shopping for a collagen product. This process breaks the collagen down into smaller peptides. Pick for well-known brands that have their products tested for contaminants and purity. For marine collagen, ensure the source is trustworthy to avoid potential issues like mercury.
Foods that Naturally Contain Collagen
If you would rather not take supplements, there are plenty of natural food sources that can help you meet your collagen needs.
- Bone broth: Rich in collagen, it’s a nourishing option that can be sipped alone or used as a base for soups.
- Chicken skin: A tasty source when prepared as part of a meal.
- Fish with skin: Provides collagen along with healthy fats, like omega-3s.
- Gelatin-based foods: Think homemade jellies or desserts made with gelatin from animal sources.
The Role of Collagen in Postpartum
A study on whether can you take collagen while breastfeeding, starting in the third trimester and continuing for 10 weeks postpartum, highlights the benefits of collagen in the postpartum period. Some key benefits include the following.
1.Wound Healing and Tissue Repair
The study showed that collagen protein supplementation led to a significant improvement in the rates of healing postpartum wounds. This is necessary for repairing wounds from childbirth, such as caesarean section incisions, vaginal tears, and episiotomy. In addition to minerals like calcium, zinc, and copper, the hydrolyzed collagen products utilized in the research also include vitamins A, C, E, and D. These vital nutrients significantly facilitate the healing of damage, angiogenesis (the formation of new blood vessels), and the maturation and stabilization of collagen.
2.General Recovery and Quality of Life
The mothers who received collagen while breastfeeding had improved overall quality of life scores, according to the study. This finding supports the idea that adequate protein intake (and, therefore, collagen supplementation) may contribute to the overall well-being and recovery of the postpartum mother.
3.Bone Health and Joint Stress:
Since bone problems may persist during the transition from pregnancy to puerperium, collagen supplementation helps support bone and joint health during this period.
4.Skin Elasticity and Abdominal Recovery
Collagen is great for skin elasticity and supports abdominal toning during pregnancy. Particularly due to its ability to preserve the skin's moisture equilibrium, collagen supplements are indispensable during pregnancy.
5.Hair and Nail Health
Some collagen supplements contain additional ingredients such as zinc and biotin that are beneficial for hair and nail growth. Given the hair loss and nail changes many women experience during the puerperium, collagen supplements containing such ingredients may help with these common postpartum problems.

Can I Take Collagen While Breastfeeding?
Many new mothers wonder, "Can I take collagen while breastfeeding?" research suggests collagen supplements are generally safe and may support postpartum recovery. Scientific studies on postpartum and breastfeeding women have found that there are no negative effects in terms of neonatal problems. The findings may be reassuring for breastfeeding mothers and health professionals using collagen supplements.
Important Considerations and Disclaimer
Always check with your primary care physician, antenatal specialist, or other healthcare provider before taking collagen supplements while pregnant or during the puerperium. Collagen supplements are normally safe to take, but it is important to remember that everyone's health is unique. Particularly in cases of preexisting conditions or other health issues, a doctor's approval is paramount. Provide your physician with the brand, ingredients, and label of the collagen product you intend to utilize.
Conclusion
As a result, taking collagen supplements during pregnancy and the postpartum period can provide many benefits, including supporting the baby's development, boosting the expectant mother's protein levels, accelerating wound healing, maintaining skin elasticity, and strengthening joint health.
Research shows that hydrolyzed collagen is generally safe and does not pose serious risks. However, it is important to choose quality products and consult your doctor before using them. By choosing trusted brands, checking the ingredients, and discussing possible interactions with your doctor, you can safely add collagen to your pregnancy and breastfeeding, supporting your health and your baby's well-being.
SOURCES
(1) - Baginski, L., Winter, M., Bailey, T. S., Capobianco, S., Granese, M., Granger, F., Miller, K., Price, K., Ramirez, S., Salcido, C., Turner, F., & O’Toole, M. (2016). Response to Hydrolysed Collagen Protein Supplementation in a Cohort of Pregnant and Post‑Partum Women. Journal of Pregnancy and Child Health, 3(5), 275.
(2) - Shi JW, Lai ZZ, Yang HL, Yang SL, Wang CJ, Ao D, Ruan LY, Shen HH, Zhou WJ, Mei J, Fu Q, Li MQ. Collagen at the maternal-fetal interface in human pregnancy. Int J Biol Sci. 2020 May 25;16(12):2220-2234. doi: 10.7150/ijbs.45586. PMID: 32549767; PMCID: PMC7294936.
Scientifically Reviwed by Omer (Matt) Sermet